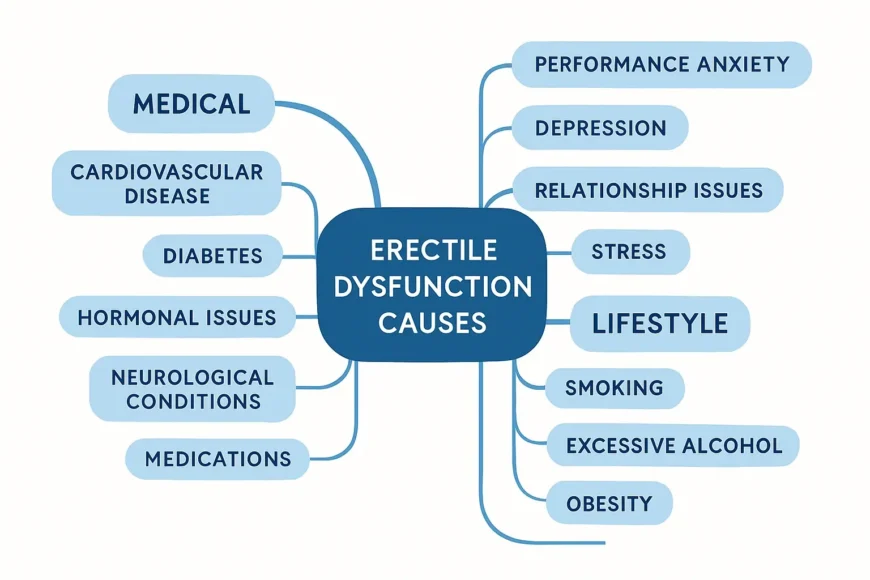
Erectile Dysfunction Causes
Erectile dysfunction affects millions of men worldwide, yet many suffer in silence due to embarrassment or lack of understanding about this treatable condition. As a practicing physician specializing in men’s health, I’ve witnessed firsthand how ED can impact not just physical intimacy but overall quality of life, relationships, and mental health.
The good news? Understanding the underlying causes is the first crucial step toward effective treatment. ED isn’t just “part of getting older” – it’s often a symptom pointing to other health issues that deserve attention.
What Exactly Is Erectile Dysfunction
Erectile dysfunction is the consistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance. Occasional difficulty with erections is normal and happens to most men at some point. However, when this becomes a persistent pattern occurring in more than 25% of sexual encounters, it’s time to seek medical evaluation.
The process of achieving an erection involves a complex coordination of psychological, neurological, hormonal, and vascular systems. When any component of this intricate process malfunctions, ED can result.
The Physical Causes: When Biology Gets in the Way
Cardiovascular Disease: The Silent Connection
The link between heart health and erectile function is stronger than many realize. Your penis serves as an early warning system for cardiovascular problems. The penile arteries are smaller than the coronary arteries, so they often show signs of blockage first.
Atherosclerosis – the buildup of plaque in arteries – restricts blood flow throughout the body, including to the penis. High blood pressure damages blood vessel walls over time, making them less elastic and reducing their ability to dilate properly during arousal.
Research shows that men with ED are 80% more likely to develop heart disease within five years. This isn’t a coincidence – it’s your body sending an important message about your overall vascular health.
Diabetes: The Sugar Connection
Diabetes represents one of the most significant risk factors for ED, affecting approximately 75% of diabetic men at some point. High blood sugar levels damage both blood vessels and nerves essential for normal erectile function.
The damage occurs gradually. Elevated glucose levels cause inflammation in blood vessel walls, leading to reduced blood flow. Simultaneously, diabetic neuropathy affects the nerves responsible for triggering and maintaining erections.
Men with poorly controlled diabetes often experience Erectile Dysfunction Symptoms 10-15 years earlier than their non-diabetic counterparts. However, good glucose control can significantly reduce this risk and sometimes reverse early erectile problems.
Hormonal Imbalances: More Than Just Testosterone
While testosterone gets most of the attention, several hormones influence erectile function:
Testosterone Deficiency (Low T): Affects libido, energy levels, and the ability to achieve firm erections. Normal levels range from 300-1000 ng/dL, but symptoms can occur even within this range if levels drop significantly from an individual’s baseline.
Thyroid Disorders: Both hyperthyroidism and hypothyroidism can disrupt sexual function. Thyroid hormones regulate metabolism and affect blood flow patterns throughout the body.
Prolactin Elevation: High prolactin levels, often caused by pituitary tumors or certain medications, suppress testosterone production and directly impact erectile function.
Neurological Conditions: When Signals Get Disrupted
The nervous system plays a crucial role in erectile function. Conditions affecting nerve pathways can interrupt the signals necessary for normal erections:
- Multiple Sclerosis: Affects up to 90% of men with MS due to nerve damage
- Parkinson’s Disease Impacts both the neurological and vascular components
- Spinal Cord Injuries: Depending on location and severity, they can partially or completely interrupt nerve signals
- Stroke: May affect the brain regions controlling sexual response
Medication Side Effects: Unintended Consequences
Many commonly prescribed medications can contribute to ED. The challenge lies in balancing necessary medical treatment with quality of life concerns.
Blood Pressure Medications: Beta-blockers and diuretics are frequent culprits, though ACE inhibitors typically have less impact on sexual function.
Antidepressants: SSRIs (Selective Serotonin Reuptake Inhibitors) can significantly impact sexual function in 30-60% of users. The effect often improves over time, but switching medications might be necessary.
Antihistamines: Over-the-counter allergy medications can reduce blood flow and affect nerve signals when used regularly.
Prostate Medications: Alpha-blockers used for enlarged prostate can cause retrograde ejaculation and sometimes ED.
Psychological Factors: The Mind-Body Connection
Performance Anxiety: The Vicious Cycle
Performance anxiety creates a self-perpetuating cycle that can transform occasional erectile difficulties into persistent problems. Initial concerns about sexual performance trigger stress responses that actually inhibit the physiological processes necessary for erections.
The sympathetic nervous system, activated during stress, constricts blood vessels and interferes with the relaxation required for blood flow to the penis. This creates a feedback loop where anxiety about ED causes the very problem it fears.
Depression and Mental Health
Depression affects erectile function through multiple pathways. The condition itself alters brain chemistry, reducing interest in pleasurable activities, including sex. Additionally, depression often involves fatigue, poor self-image, and decreased motivation – all factors that impact sexual function.
Chronic stress elevates cortisol levels, which suppresses testosterone production. The relationship works both ways: ED can contribute to depression, creating a complex cycle that requires comprehensive treatment addressing both conditions.
Relationship Issues: Beyond the Physical
Relationship problems often manifest in the bedroom. Unresolved conflicts, communication issues, or loss of emotional intimacy can translate into physical sexual difficulties. The stress of relationship problems activates the same physiological responses that interfere with erectile function.
Past traumatic experiences, whether sexual or otherwise, can create psychological barriers to sexual function. These issues require sensitivity and often benefit from professional counseling support.
Lifestyle Factors: Choices That Matter
Smoking: The Hidden Enemy
Smoking damages blood vessels throughout the body, including those supplying the penis. Nicotine constricts blood vessels immediately, while long-term smoking causes permanent vascular damage through atherosclerosis.
Studies show that men who smoke are twice as likely to experience ED compared to non-smokers. The good news is that quitting smoking can improve erectile function relatively quickly – often within weeks to months.
Alcohol: The Double-Edged Sword
Moderate alcohol consumption might actually have some cardiovascular benefits, but excessive drinking is detrimental to sexual function. Alcohol is a depressant that affects the central nervous system’s ability to coordinate the complex process of achieving an erection.
Chronic heavy drinking can lead to permanent nerve damage, hormonal imbalances, and liver disease – all of which contribute to ED. Even binge drinking episodes can temporarily disrupt erectile function for days afterward.
Obesity: The Metabolic Impact
Excess weight contributes to ED through several mechanisms:
- Vascular Effects: Obesity promotes atherosclerosis and reduces blood flow
- Hormonal Changes: Fat tissue converts testosterone to estrogen, lowering available testosterone
- Inflammation: Chronic low-grade inflammation associated with obesity damages blood vessels
- Insulin Resistance: Often precedes diabetes and affects vascular function
Research indicates that men with a BMI over 30 have a 30% higher risk of ED compared to men with healthy weights. Weight loss through diet and exercise can significantly improve erectile function.
Sleep Disorders: The Overlooked Factor
Quality sleep is essential for hormonal balance. Testosterone production peaks during deep sleep stages, and chronic sleep deprivation can reduce testosterone levels by 10-15%.
Sleep apnea, affecting up to 69% of men with ED, creates a double problem. The condition disrupts sleep quality and testosterone production while also affecting cardiovascular health through repeated oxygen deprivation episodes.
Age-Related Changes: Understanding Normal Aging
While ED isn’t an inevitable part of aging, certain age-related changes do affect sexual function:
Vascular Changes: Blood vessels naturally become less elastic with age, though healthy lifestyle choices can minimize this effect.
Hormonal Shifts: Testosterone levels typically decline by 1-2% annually after age 40, though this varies significantly between individuals.
Medication Accumulation: Older adults often take multiple medications, increasing the likelihood of drug-related sexual side effects.
Chronic Conditions: The prevalence of diabetes, heart disease, and other ED-contributing conditions increases with age.
However, many men maintain satisfactory sexual function well into their 80s and beyond. Age alone shouldn’t be accepted as an explanation for erectile problems.
Medical Conditions That Contribute to ED
Prostate Problems
Benign prostatic hyperplasia (enlarged prostate) and prostate cancer treatments can affect erectile function. Surgical procedures, radiation therapy, and hormone treatments for prostate cancer carry varying risks of ED, though nerve-sparing techniques have improved outcomes significantly.
Kidney Disease
Chronic kidney disease affects erectile function through multiple pathways, including vascular damage, hormonal imbalances, and medication side effects. Dialysis patients experience ED rates of 70-90%.
Liver Disease
The liver plays a crucial role in hormone metabolism. Liver disease can lead to decreased testosterone production and increased estrogen levels, both contributing to erectile dysfunction.
The Interconnected Web: Understanding Complex Causes
Rarely does ED result from a single cause. Most men experience a combination of factors working together. A 55-year-old man with mild diabetes, moderate stress, and a prescription for blood pressure medication might develop ED from the cumulative effect of these factors, even though none alone would necessarily cause problems.
This complexity explains why effective treatment often requires a comprehensive approach addressing multiple contributing factors simultaneously.
Red Flags: When to Seek Immediate Medical Attention
Certain symptoms accompanying ED warrant urgent evaluation:
– Sudden onset of ED in previously healthy men
– ED following trauma or injury
– Curved or bent penis during erection (possible Peyronie’s disease)
– Loss of morning erections
– ED accompanied by chest pain, shortness of breath, or other cardiac symptoms
– Signs of hormonal deficiency (fatigue, mood changes, muscle loss)
The Evaluation Process: What to Expect
A thorough medical evaluation typically includes:
Medical History: Discussion of symptoms, timing, associated factors, medications, and overall health status.
Physical Examination: Assessment of cardiovascular health, genital examination, and evaluation for signs of hormonal deficiency.
Laboratory Tests: Blood work checking testosterone levels, glucose, cholesterol, and other relevant markers.
Specialized Testing: In some cases, additional tests like penile ultrasound or nocturnal erection monitoring may be recommended.
Treatment Implications: Matching Solutions to Causes
Understanding the underlying cause guides treatment selection:
Vascular Causes: Often respond well to PDE5 inhibitors (Viagra, Cialis) or vascular interventions.
Hormonal Causes: May require hormone replacement therapy or treatment of underlying endocrine disorders.
Psychological Causes: Benefit from counseling, stress management, or changes in antidepressant medications.
Lifestyle-Related Causes: Respond to modifications in diet, exercise, smoking cessation, or alcohol reduction.
Prevention Strategies: Protecting Your Sexual Health
Many ED causes are preventable through lifestyle modifications:
Maintain Cardiovascular Health: Regular exercise, a healthy diet, blood pressure control, and cholesterol management protect both heart and sexual health.
Manage Diabetes: Keep blood sugar levels well-controlled through diet, exercise, and appropriate medication.
Exercise Regularly: Physical activity improves blood flow, reduces stress, and helps maintain a healthy weight. Kegel exercises specifically strengthen pelvic floor muscles important for erectile function.
Limit Alcohol: Moderate consumption (no more than two drinks daily) minimizes the risk of alcohol-related ED.
Don’t Smoke: If you smoke, quitting is one of the most impactful steps you can take for sexual health.
Manage Stress: Develop healthy coping mechanisms through exercise, meditation, hobbies, or professional counseling.
Prioritize Sleep: Aim for 7-9 hours of quality sleep nightly to support hormonal balance.
The Role of Communication
Discussing ED with your healthcare provider shouldn’t be embarrassing. We’re medical professionals who understand that sexual health is an important component of overall well-being. The more honest and detailed information you provide, the better we can help identify causes and develop effective treatment plans.
Similarly, open communication with your partner about sexual concerns can reduce performance anxiety and strengthen your relationship during the treatment process.
Looking Forward: Hope and Solutions
Erectile dysfunction is highly treatable regardless of the underlying cause. Modern medicine offers numerous effective options, from lifestyle modifications and counseling to medications, devices, and surgical interventions.
The key is accurate diagnosis of contributing factors. What works for one man might not work for another because the underlying causes differ. This is why cookie-cutter approaches often fail, and individualized treatment plans based on thorough evaluation produce the best results.
Remember that seeking help for ED often uncovers other health issues that need attention. Many of my patients discover and address cardiovascular problems, diabetes, or hormonal imbalances during their ED evaluation. In this way, addressing sexual health concerns can actually improve overall health and longevity.
Taking the Next Step
If you’re experiencing persistent erectile difficulties, don’t wait for the problem to resolve on its own. Early intervention typically leads to better outcomes and may prevent progression of underlying health conditions.
Schedule an appointment with your primary care physician or a specialist in men’s health. Come prepared to discuss your symptoms honestly, including their duration, severity, and any patterns you’ve noticed. Bring a list of all medications and supplements you’re taking.
Sexual health is an integral part of overall well-being. You deserve comprehensive, compassionate care that addresses not just the symptoms, but the underlying causes of erectile dysfunction. With proper evaluation and Erectile Dysfunction Treatment, most men can return to satisfying sexual function and improved quality of life.
The journey to better sexual health begins with understanding. Armed with knowledge about potential causes, you’re better equipped to work with your healthcare provider in developing an effective treatment strategy tailored to your specific situation.
FAQs
Can lifestyle changes improve ED?
Yes, lifestyle improvements such as quitting smoking, reducing alcohol intake, losing weight, eating a healthy diet, increasing physical activity, and improving sleep can help reduce ED risk and severity.
Which medical conditions are commonly linked to ED?
Chronic conditions like heart disease, diabetes, high blood pressure, and hormonal imbalances (such as low testosterone) are strongly associated with erectile dysfunction.
Does ED only affect older men?
While ED is more common in older men, it can affect adults of any age due to medical conditions, psychological issues, or lifestyle factors.
When should I seek medical advice for ED?
If ED is ongoing, interferes with your relationships, or causes emotional distress, it’s important to consult a healthcare provider. ED could be a sign of underlying health problems that need to be addressed.
If I have ED, does that mean I’m going to have a heart attack?
Not necessarily, but ED can be an early warning sign of cardiovascular problems. The arteries in the penis are smaller than those around the heart, so they often show signs of blockage first. Studies show that men with ED are at higher risk for heart disease, but this doesn’t mean a heart attack is imminent.
Will my ED go away if I lose weight?
Weight loss can significantly improve erectile function, especially if obesity is a contributing factor. Losing even 10% of your body weight can make a meaningful difference. Here’s why:
– Improved blood flow as cardiovascular health improves
– Higher testosterone levels (fat tissue converts testosterone to estrogen)
– Reduced inflammation throughout the body
– Better insulin sensitivity
– Improved self-confidence and energy levels
References

Board-Certified Urologist | Male Reproductive Specialist | Associate Professor of Urology
Dr. Matt Coward is an ABMS board-certified urologist with over 10 years of experience and specialized expertise in male reproductive health and infertility. He currently serves as the Director of Male Reproductive Medicine and Surgery at UNC Fertility in Raleigh, North Carolina, and is the Fellowship Director of the UNC Men’s Health Fellowship.







