Erectile Dysfunction Treatment
In 30 Seconds…
Erectile Dysfunction treatment isn’t one-size-fits-all — it depends on what’s causing the problem. Some men respond well to lifestyle changes like better sleep, exercise, and quitting smoking. Others may need medications such as sildenafil (Viagra) or tadalafil (Cialis), or advanced options like shockwave therapy or penile injections.
Introduction
Erectile dysfunction treatment is most effective when tailored to the cause, starting with lifestyle and oral medications and escalating to devices, injections, or implants when needed. Evidence-based guidelines emphasize shared decision-making, transparent discussion of risks and benefits, and consideration of psychological, hormonal, and cardiovascular factors that often drive erectile difficulties.
What Erectile Dysfunction is
Erectile dysfunction (ED) is the persistent inability to achieve or maintain an erection adequate for satisfactory sexual activity, and it reflects vascular, neurologic, hormonal, and psychogenic influences rather than a single disease. Prevalence increases with age and cardiometabolic comorbidity, and the condition often overlaps with cardiovascular risk, diabetes, obesity, sleep apnea, depression, and medication effects.
Because ED can be an early marker of endothelial dysfunction, clinicians use ED as a prompt to assess blood pressure, lipids, glucose, and overall heart health while addressing sexual function directly.
How ED is Evaluated
An effective evaluation combines medical and sexual history, focused physical exam, medication review, mental health screening, and selective labs such as fasting glucose or HbA1c, lipids, and morning testosterone when hypogonadism is suspected. Guidelines support assessing relationship dynamics and performance anxiety and considering referral to a mental health professional to improve adherence and outcomes.
Specialized testing—penile Doppler ultrasound, nocturnal tumescence testing, or neurologic assessment—is reserved for complex cases, post-surgical states, or when invasive therapies are planned.
First-Line treatments
For most men, first-line care includes addressing lifestyle, optimizing comorbidities, and offering an FDA‑approved oral phosphodiesterase type‑5 inhibitor (PDE5i) unless contraindicated. Smoking cessation, exercise, weight loss, and treatment of sleep apnea and depression can improve erectile function and reduce cardiovascular risk simultaneously.
PDE5 inhibitors—sildenafil, tadalafil, vardenafil, and avanafil—enhance nitric oxide–cGMP signaling in penile smooth muscle, improving rigidity with sexual stimulation, and differ mainly in onset, duration, and side-effect profiles.
When Pills aren’t Enough
About one-third of men do not achieve satisfactory erections with PDE5 inhibitors alone due to the severity of vascular disease, diabetes, neuropathy, or incorrect use. After reviewing technique and timing, second-line options include vacuum erection devices, intraurethral alprostadil, and intracavernosal injections that directly induce cavernosal smooth muscle relaxation. Vacuum erection devices create negative pressure to draw blood into the corpora cavernosa and, with a constriction ring, can restore functional erections for many couples without systemic side effects.
Devices that work
Vacuum erection devices (VEDs) have high success and satisfaction rates with minimal systemic risk, though some users report bruising, coldness, or constriction ring discomfort. As a rehabilitation tool after prostate surgery, regular VED use supports oxygenation of the corpora cavernosa and helps counteract disuse atrophy. In men who cannot take PDE5 inhibitors due to nitrate therapy or side effects, a VED provides a non-pharmacologic, repeatable solution at home.
Injections and urethral therapies
Alprostadil can be placed intraurethrally or injected intracavernosally, alone or in combination with papaverine and phentolamine, achieving strong erections independent of nitric oxide pathways. Intraurethral alprostadil offers a needle‑free route but is less potent than injections and may cause urethral burning, while injections require teaching but provide reliable rigidity for severe ED. Guidelines endorse these therapies as first-line alternatives when pills are contraindicated or ineffective, and as second-line when escalation is required.
Testosterone and sexual health
Men with symptoms of hypogonadism and low morning total testosterone on repeat testing may benefit from testosterone therapy, which can improve libido and augment PDE5 response in appropriately selected patients. Testosterone should not be used as a sole ED treatment in eugonadal men and requires monitoring for erythrocytosis, prostate effects, and fertility concerns. Contemporary European guidance integrates hypogonadism management with ED care to optimize sexual function while balancing safety.
Penile implants
For men who fail or decline conservative treatments, penile prostheses deliver the highest satisfaction for both patient and partner by providing on-demand rigidity. Inflatable penile prostheses allow more natural concealment and control, while malleable rods offer simplicity with fewer mechanical parts. Surgery carries risks of infection and mechanical failure and should be deferred in the presence of active infections, with careful counseling and experienced surgical care improving outcomes.
Shockwaves and regenerative options
Low-intensity extracorporeal shockwave therapy (Li‑ESWT) aims to improve penile hemodynamics via angiogenesis and remodeling, and emerging data show benefit in mild to moderate vasculogenic ED, sometimes as an adjunct to PDE5 inhibitors. Major guidelines and academic centers still classify Li‑ESWT as investigational or experimental, and it is not FDA‑approved for ED, with out‑of‑pocket costs typical in clinical practice. Patients should avoid “radial wave” offerings marketed outside medical settings because current evidence does not support their efficacy for the ED.
What’s new and what’s next
Regenerative strategies under study include stem cell–derived products, platelet‑rich plasma (PRP), exosomes, and gene therapy targeting nitric oxide and vascular pathways. Early-phase results are promising but heterogeneous, and these approaches remain research‑stage without regulatory approval or standardized protocols for routine ED care. Pipeline pharmacology includes centrally acting melanocortin and dopamine receptor agonists and next‑generation PDE5 inhibitors and delivery systems, but clinical availability for ED remains limited today.
A practical treatment ladder
Treatment selection should reflect severity, comorbidities, preferences, and partner goals, starting with risk‑factor control and oral agents, then progressing to devices or local pharmacotherapy, and finally to surgical prosthesis when durability is paramount. Mental health support improves adherence, reduces performance anxiety, and helps couples integrate therapies successfully, and should be considered at any stage.
Men with focal arterial injury after pelvic trauma and no systemic vascular disease can be considered for revascularization in select centers, while venous surgery is not recommended.
Expected outcomes and safety
PDE5 inhibitors improve erections in a majority of appropriately counseled men, with common transient side effects like flushing, nasal congestion, and headache, and strict avoidance with nitrates due to hypotension risk. Injection therapy and intraurethral alprostadil yield robust erections in many PDE5‑nonresponders, with priapism and fibrosis risks mitigated by dosing protocols and follow‑up.
Penile implants achieve high satisfaction across etiologies of ED, but require informed consent regarding infection prevention, revision rates, and the irreversible nature of corporal implantation.
Special Situations
Diabetes, post‑prostatectomy states, Peyronie’s disease, spinal cord injury, and pelvic radiation demand tailored plans that may combine rehabilitation, device therapy, and surgical options. Penile rehabilitation strategies often include early VED use, PDE5 agents when feasible, and intracavernosal training to preserve tissue health while neural recovery occurs.
When curvature from Peyronie’s disease coexists with ED, sequencing of plaque treatment and implant considerations should be individualized to restore both straightness and rigidity.
Counseling on expectations
Clear guidance on the timing of medications with sexual activity, the need for stimulation with PDE5 inhibitors, and the stepwise nature of care prevents premature abandonment of effective therapies. Discussions should include the impact of alcohol, recreational drugs, and antihypertensives or antidepressants on erectile function, and whether substitutions are possible.
Partner involvement improves satisfaction, reduces anxiety, and aligns goals for spontaneity, sensation, and reliability, which can influence the choice between pharmacologic and device-based solutions.
Treatment tiers and typical use
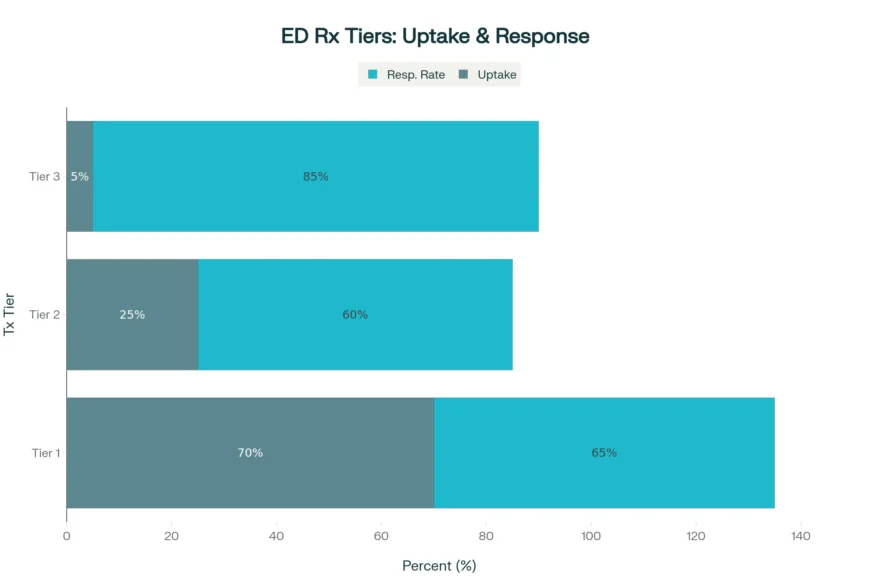
A three-tier horizontal bar chart in blue shows the proportion of men who typically respond or choose each step over time, acknowledging variability across studies.
- Tier 1: Lifestyle + PDE5 inhibitors — broad first use; majority trial; moderate-to-high response in appropriate candidates.
- Tier 2: VED, intraurethral alprostadil, intracavernosal injections — second-line uptake; good efficacy in PDE5 nonresponders.
- Tier 3: Penile prosthesis — smaller share, highest satisfaction in refractory ED.
Cost and access
Most oral agents are available generically and are widely covered, while Li‑ESWT is cash‑pay and typically delivered in six or more sessions, costing several hundred dollars each. Insurance coverage generally supports VEDs and surgery after failure of conservative therapy, with prior authorization often required for implants.
Telemedicine has improved access to evaluation and prescription therapy, but in‑person assessment is crucial when symptoms suggest hypogonadism, Peyronie’s disease, or cardiovascular red flags.
Red flags that need attention
New-onset ED with exertional symptoms, chest pain, or claudication warrants cardiovascular evaluation because penile arteries are sensitive indicators of systemic vascular disease.
Marked loss of morning erections with low libido and fatigue suggests hypogonadism and should prompt testosterone testing and endocrine review. Painful curvature, sudden deformity, or a palpable plaque suggests Peyronie’s disease and change treatment priorities and timelines.
Evidence and guidelines at a glance
Authoritative guidance emphasizes offering all appropriate options—regardless of invasiveness—through shared decision-making, with mental health and lifestyle counseling embedded in care. Recent European and national recommendations broaden second-line choices, endorse vacuum therapy broadly, and permit Li‑ESWT consideration in mild to moderate ED while recognizing the investigational status in many regions.
Ongoing research continues to refine regenerative therapies and next‑generation drugs, but today’s durable solution for refractory cases remains the penile prosthesis.
Closing thoughts
ED is treatable at every stage, and outcomes are best when cardiovascular health, hormones, mental well‑being, and relationship context are addressed alongside targeted sexual-function therapies.
A structured ladder—optimize health, try oral agents correctly, add devices or local pharmacotherapy, and move to implants when needed—restores confidence and intimacy for most men. For novel therapies, seek centers conducting trials or offering evidence‑based protocols, and be cautious of non‑medical claims that overpromise results without regulatory oversight.
FAQs
What are the first treatments most men try?
Most men begin with lifestyle optimization—exercise, weight management, smoking cessation, sleep apnea treatment—and an oral phosphodiesterase‑5 inhibitor (PDE5 inhibitor) like sildenafil or tadalafil, assuming no contraindications such as nitrate use. These medications enhance nitric oxide–cGMP signaling to improve penile blood flow with sexual stimulation, and differ mainly in onset and duration.
What if oral medications do not work?
If correct dosing and timing are confirmed and erections remain unsatisfactory, effective next steps include vacuum erection devices (VEDs), intraurethral alprostadil, or intracavernosal injections that directly relax cavernosal smooth muscle. About one‑third of men may not respond adequately to pills due to factors like severe vascular disease, neuropathy, or diabetes, making device‑based or local therapies valuable options.
Are vacuum erection devices safe and effective?
Yes, VEDs are generally safe, medication‑free, and effective, creating negative pressure to draw blood into the penis and a constriction ring to maintain the erection, though some men report bruising, coolness, or ring discomfort. VEDs are also used for penile rehabilitation after prostate surgery to support oxygenation and help limit disuse atrophy.
When is testosterone therapy appropriate?
Testosterone therapy is considered when men have symptoms of hypogonadism and consistently low morning total testosterone on repeat testing, and it can improve libido and sometimes PDE5 response when low T overlaps with ED. It is not a primary ED treatment for men with normal testosterone and requires monitoring for erythrocytosis, prostate parameters, and effects on fertility.
What red flags need immediate attention?
Sudden ED with exertional chest pain or breathlessness, marked loss of morning erections with low libido and fatigue suggestive of hypogonadism, or painful curvature and palpable plaques indicating Peyronie’s disease all warrant prompt evaluation. Any prolonged erection lasting more than four hours (priapism) after injection therapy is an emergency and requires urgent care.
How should treatment be sequenced for best results?
A practical ladder begins with risk‑factor control and correct use of oral agents, progresses to VEDs or local pharmacotherapy if needed, and moves to penile prosthesis for a durable, reliable solution when conservative measures are insufficient. Mental health support and partner engagement can improve adherence, satisfaction, and overall outcomes at every step.
References

Board-Certified Urologist | Male Reproductive Specialist | Associate Professor of Urology
Dr. Matt Coward is an ABMS board-certified urologist with over 10 years of experience and specialized expertise in male reproductive health and infertility. He currently serves as the Director of Male Reproductive Medicine and Surgery at UNC Fertility in Raleigh, North Carolina, and is the Fellowship Director of the UNC Men’s Health Fellowship.







