Can a Toothache Cause a Headache?
In 30 seconds…
Yes, a toothache can cause a headache.
This happens because teeth and the head share the same nerves, especially the trigeminal nerve. Dental problems like cavities, tooth infections, gum disease, or impacted wisdom teeth can send pain signals to the head, temples, or behind the eyes, resulting in a headache. Treating the tooth problem usually relieves the headache.
Introduction
Have you ever experienced a throbbing toothache that seemed to spread into your temples, forehead, or even the back of your head? You’re not alone. Many people wonder: can a toothache cause a headache? The answer is yes—dental problems can absolutely trigger or worsen headaches. The connection lies in shared nerve pathways and the way pain signals travel through your face and skull. When tooth pain radiates beyond the mouth, it can be difficult to pinpoint whether you’re dealing with a dental issue, a headache disorder, or both.
Understanding this tooth pain and headache connection is crucial for getting the right treatment. In this guide, we’ll explore how dental problems like infections, nerve inflammation, and jaw disorders can lead to head pain. You’ll learn to recognize the warning signs, understand the biological mechanisms at play, and discover effective ways to find relief. Whether you’re dealing with a sudden toothache or chronic facial pain, knowing the link between your oral health and headaches can help you take the right steps toward lasting comfort.
How Are Toothaches and Headaches Connected?
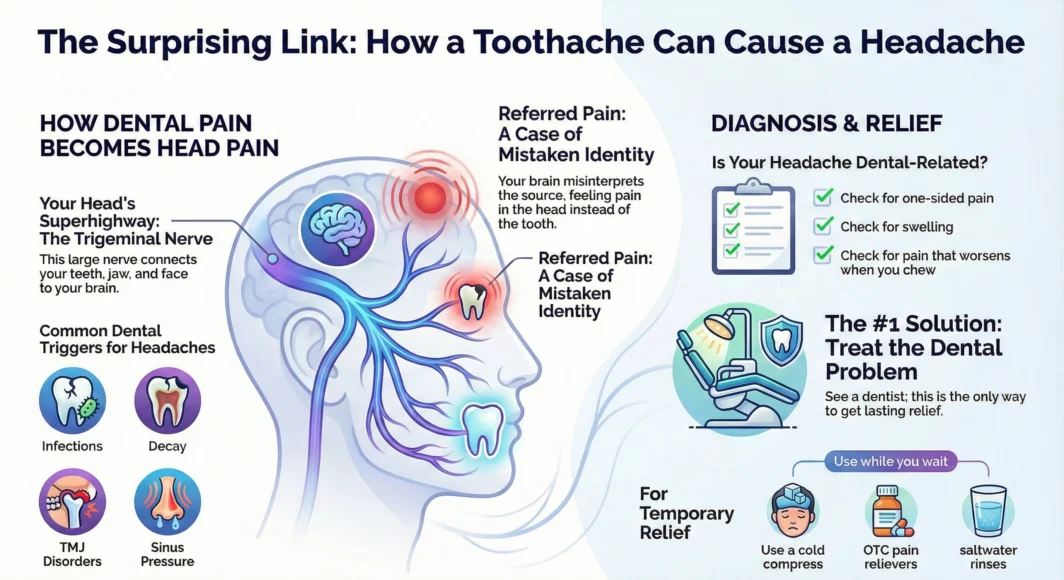
The connection between toothaches and headaches isn’t coincidental—it’s rooted in your body’s nerve anatomy. The trigeminal nerve, the largest cranial nerve in your head, serves as the primary bridge between oral pain and head pain. This nerve has three major branches that transmit sensation from your face, teeth, jaw, and head to your brain. When one area becomes inflamed or irritated, the pain signals can spread along these interconnected pathways.
This phenomenon is called referred pain, where your brain misinterprets the origin of discomfort. Because the trigeminal nerve carries signals from both your teeth and various parts of your head, inflammation in one area can trigger pain perception in another. For example, an infected lower molar might send pain signals that your brain registers as a temple headache or vice versa. This tooth nerve pain and migraine relationship explains why dental issues often present with confusing pain patterns that seem to move or radiate beyond the original source.
Common Dental Problems That Can Trigger Headaches
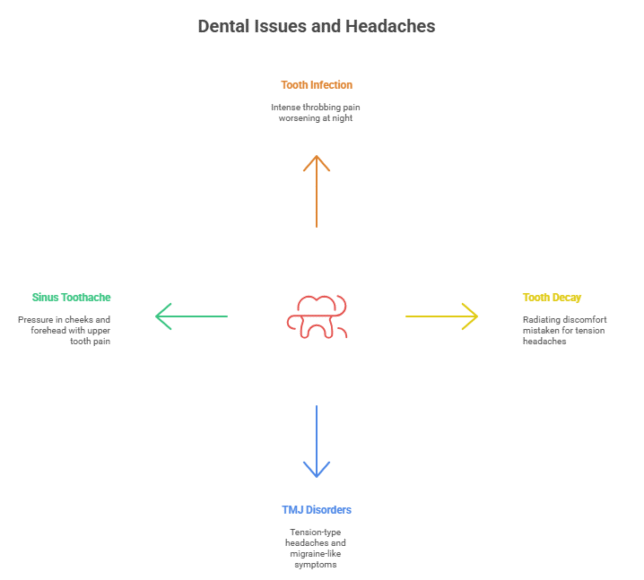
Tooth Infection or Abscess
A tooth infection or dental abscess occurs when bacteria invade the inner pulp of your tooth, creating a pocket of pus and pressure. This infection doesn’t stay confined to the tooth—as pressure builds, pain signals radiate along nerve pathways to your jaw, temples, and forehead. Can a tooth infection cause a headache? Absolutely. The inflammatory response triggers intense throbbing that often worsens at night or when lying down. Left untreated, the infection can spread to surrounding tissues, intensifying both the toothache and accompanying headache.
Tooth Decay or Nerve Inflammation
When tooth decay penetrates through the enamel and reaches the inner pulp chamber, it exposes sensitive nerve endings to bacteria and temperature changes. This inflamed pulp sends constant pain signals through the trigeminal nerve network. The result is not just localized tooth sensitivity, but radiating discomfort that manifests as facial pain and headaches. As nerve irritation intensifies, the pain can spread from the tooth to your cheek, jaw, and eventually your temples or forehead, creating a persistent ache that many people mistake for tension headaches.
TMJ (Temporomandibular Joint) Disorders
The temporomandibular joint connects your jawbone to your skull, and when this joint becomes misaligned or strained, it creates a cascade of pain throughout your face and head. TMJ disorders often result from teeth grinding, jaw clenching, poor bite alignment, or injury. The jaw pain and headache link is particularly strong with TMJ because the constant muscle tension affects the trigeminal nerve and surrounding structures. People with TMJ frequently experience tension-type headaches, pain behind the eyes, and even migraine-like symptoms that can be debilitating and chronic.
Sinus Toothache and Pressure Headaches
Your upper back teeth share a close relationship with your maxillary sinuses—the air-filled spaces in your cheekbones. When sinuses become infected or inflamed, the pressure can affect the roots of your upper molars, creating what’s known as a sinus toothache. The reverse is also true: an infected upper tooth can trigger sinus inflammation. This creates the classic sinus toothache headache presentation: pressure in your cheeks and forehead, pain that worsens when bending forward, and discomfort in your upper teeth. The pain often affects multiple teeth on one side rather than a single tooth.
Symptoms That Indicate Your Headache Might Be Dental-Related
Recognizing the signs of dental pain causing headache can help you seek the right treatment faster:
- Pain increases when chewing or biting: If your headache intensifies while eating or applying pressure to specific teeth, a dental issue is likely the culprit.
- One-sided facial or jaw pain: Headaches stemming from tooth problems typically affect one side of your face, corresponding to the location of the dental issue.
- Swelling or tenderness near a tooth: Visible signs of infection, gum inflammation, or facial swelling alongside your headache strongly suggest a dental origin.
- Headache improves after dental treatment: If your chronic headaches significantly decrease after getting a filling, root canal, or tooth extraction, the tooth problem was likely triggering your head pain.
Identifying the root cause is essential for preventing chronic headaches. Many people take pain medication for what they assume are regular headaches, only to find temporary relief because the underlying dental problem remains untreated. If you notice these patterns, scheduling a dental examination can reveal hidden infections, decay, or jaw issues that standard headache treatments won’t resolve.
How Tooth Nerve Pain Can Trigger Migraines
The connection between tooth nerve pain and migraine goes beyond simple pain referral—it involves complex neurological mechanisms. When dental problems cause prolonged inflammation or nerve irritation, they create overstimulation of the trigeminal nerve pathways. This nerve is directly connected to the brainstem and several pain-processing centers in the brain. In individuals who are predisposed to migraines, this constant trigeminal nerve activation can lower the threshold for migraine attacks.
Research has shown that dental pain may activate the same neurological pathways involved in migraine generation. The trigeminal nerve can trigger the release of inflammatory substances called neuropeptides, which dilate blood vessels and sensitize pain receptors throughout the head. For people with existing migraine conditions, unresolved dental issues can increase both the frequency and intensity of their migraine episodes. Some patients report that after treating an infected tooth or addressing TMJ problems, their long-standing migraines significantly improved or disappeared entirely.
Headache After Dental Work — Normal or Concerning?
Experiencing a headache after dental work is relatively common and usually temporary. Several factors can contribute to post-dental headaches:
- Anesthesia wear-off: As the numbing medication fades, you may feel throbbing or aching around the treatment site that radiates to your head.
- Jaw strain: Keeping your mouth open for extended periods during dental procedures can strain your jaw muscles and trigger tension headaches.
- Stress and anxiety: Dental anxiety can cause muscle tension in your neck, shoulders, and jaw, leading to stress headaches after your appointment.
- Inflammatory response: Your body’s natural healing response to dental work involves some inflammation, which can temporarily cause discomfort.
Most headaches after dental work should resolve within 24-48 hours. However, you should contact your dentist if you experience severe, worsening pain, fever, significant swelling, or headaches that persist beyond a few days. These symptoms could indicate complications like infection or dry socket. If your headache is accompanied by vision changes, confusion, or severe nausea, seek medical attention immediately as these aren’t typical post-dental symptoms.
How to Relieve Headaches Caused by a Toothache
Addressing both the dental issue and the headache symptoms provides the most effective relief:
Treat the Underlying Dental Problem: This is the most important step. Schedule a dental appointment to address infections, decay, or structural issues. Treatments may include antibiotics for infections, fillings for cavities, root canals for nerve damage, or dental appliances for TMJ disorders.
Apply a Cold Compress: Place an ice pack wrapped in a thin cloth on your jaw or cheek for 15-20 minutes at a time. This reduces inflammation and numbs pain signals traveling to your head.
Over-the-Counter Pain Relief: Ibuprofen or acetaminophen can provide temporary relief from both tooth pain and headaches. Always follow dosage instructions and consult your doctor if you have any health conditions.
Reduce Clenching and Grinding: Be mindful of jaw tension throughout the day. Consciously relax your jaw muscles, keeping your teeth slightly apart when not eating or speaking.
Stay Hydrated: Dehydration can worsen headaches. Drinking plenty of water supports your body’s healing processes and may reduce pain intensity.
Natural Remedies
While not substitutes for professional dental care, these approaches can provide additional comfort:
- Saltwater rinse: Mix half a teaspoon of salt in warm water and gently swish for 30 seconds to reduce oral bacteria and inflammation.
- Clove oil: Apply a small amount to the affected tooth using a cotton swab. Clove oil contains eugenol, a natural anesthetic and anti-inflammatory compound.
- Peppermint tea: The cooling effect and anti-inflammatory properties may soothe both dental and head pain.
- Elevation: Sleep with your head slightly elevated to reduce blood pressure in your head and decrease throbbing pain.
Prevention Tips for Avoiding Toothache Cause Headaches
Preventing dental problems is the best way to avoid the toothache and headache connection:
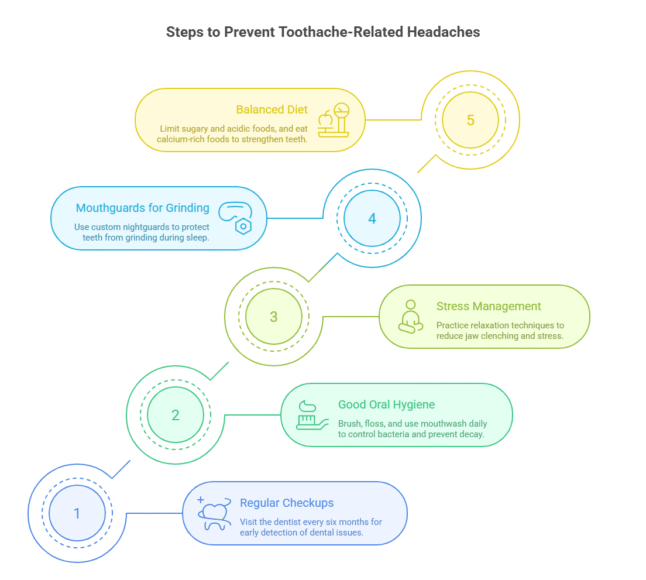
Schedule Regular Dental Checkups: Visit your dentist every six months for cleanings and examinations. Early detection of cavities, gum disease, or other issues prevents them from progressing to painful infections.
Practice Good Oral Hygiene: Brush twice daily with fluoride toothpaste, floss daily, and use antimicrobial mouthwash to keep bacteria under control and prevent decay.
Manage Stress and Jaw Clenching: Practice stress-reduction techniques like meditation, yoga, or deep breathing. If you notice yourself clenching your jaw during the day, make a conscious effort to relax.
Use Mouthguards for Grinding: If you grind your teeth at night (bruxism), ask your dentist about a custom nightguard to protect your teeth and reduce jaw strain.
Maintain a Balanced Diet: Limit sugary foods and acidic beverages that contribute to tooth decay. Eat calcium-rich foods to strengthen tooth enamel, and drink plenty of water to wash away food particles and bacteria.
Conclusion
Understanding that a toothache can cause a headache is essential for finding effective treatment and relief. The connection is more than coincidental—your teeth and head share the trigeminal nerve pathway, making pain referral between these areas common. Dental problems, including infections, decay, TMJ disorders, and sinus-related issues, can all trigger or worsen headaches that significantly impact your quality of life.
The key takeaways are clear: dental health and head pain are intimately connected, early diagnosis prevents chronic suffering, and proper dental care can eliminate headaches you’ve been living with for months or even years. Don’t dismiss persistent headaches as simply stress or tension—they may be your body’s way of signaling an underlying oral health problem.
If you’re experiencing both toothaches and headaches, take action now. Schedule an appointment with your dentist to rule out or treat dental causes, and consult with your doctor if headaches persist after dental treatment. By addressing the root cause rather than just masking symptoms, you can achieve lasting relief and prevent future episodes of dental-related head pain.
Related Articles:
FAQs
Can a cavity cause a headache?
Yes, a cavity can cause a headache, especially when it reaches the inner pulp layer of your tooth. As decay progresses deeper into the tooth structure, it triggers nerve inflammation that sends pain signals along the trigeminal nerve pathways to your head. The headache may be localized near the affected tooth or spread to your temples and forehead.
How do I know if my headache is from a tooth infection?
Several signs suggest your headache stems from a tooth infection: the pain is typically on one side of your face, worsens when chewing or lying down, and may be accompanied by dental symptoms like swelling, bad taste in your mouth, or visible gum inflammation. If you have a fever along with a headache and tooth pain, an infection is highly likely.
Can TMJ cause migraine-like headaches?
Yes, TMJ disorders can trigger headaches that closely resemble migraines. The intense jaw muscle tension and joint inflammation affect the trigeminal nerve, potentially causing severe one-sided head pain, sensitivity to light and sound, and nausea. Many people with TMJ have been misdiagnosed with primary migraine disorders before the jaw issue was identified.
Does removing a bad tooth stop headaches?
In many cases, extracting a severely infected or damaged tooth can eliminate associated headaches. Once the source of infection and inflammation is removed, the constant nerve irritation stops, and the headaches often resolve within a few days. However, if other dental issues or conditions exist, additional treatment may be necessary.
What’s the fastest way to relieve a headache from a toothache?
The fastest temporary relief comes from taking anti-inflammatory medication like ibuprofen, applying a cold compress to your jaw, and rinsing with warm saltwater. However, these only address symptoms—seeing a dentist promptly to treat the underlying dental problem provides the most effective and lasting relief.
References

Board-Certified Family Medicine Physician | HIV Specialist™ (AAHIVS) | Public Health Advocate
Dr. Avi Varma is a board-certified family medicine physician and HIV Specialist™ with over 10 years of experience in primary care, infectious disease management, and community health. Based in Atlanta, Georgia, she works with a nonprofit organization dedicated to ending the HIV epidemic. Dr. Varma holds a Master’s in Public Health from Johns Hopkins University and is a Fellow of the American Academy of Family Physicians. She is deeply committed to advancing equitable healthcare and improving outcomes for underserved populations.







